Why is pancreatic cancer called the king of cancer? Who are the high-risk groups? Understand symptoms, examinations and treatments at once
Why is pancreatic cancer called the king of cancer? Is the cause related to diet?
According to statistics on the top ten causes of cancer death in 2021, pancreatic cancer ranks seventh. Compared with ten years ago, the number of deaths from pancreatic cancer has increased by 62.7%. Its average 5-year survival rate is only 1%-4%, which is regarded as One of the cancers with the worst prognosis. Because pancreatic cancer is difficult to diagnose early, most tumors are discovered at an advanced stage, and the response to chemotherapy, radiotherapy, immunotherapy, and cell therapy is not ideal. There has been no significant progress in the diagnosis and treatment of pancreatic cancer in medicine, so it is known as the “King of Cancer” in the community.
The exact cause of pancreatic cancer is still unclear. Various lifestyle habits that may increase the risk of cancer, such as smoking, drinking, and obesity, are all considered risk factors related to pancreatic cancer. A family history of pancreatic cancer in an immediate relative is an important risk indicator. Among various related diseases, diabetes and chronic pancreatitis appear to be associated with a higher incidence of pancreatic cancer. Since the pancreas is responsible for endocrine functions, abnormal blood sugar metabolism may be a warning sign of cancer.
In addition, some studies believe that environmental or occupational exposure to various dyes and solvents can also increase the risk of pancreatic cancer. Although there is no evidence linking specific dietary habits to pancreatic cancer, drinking alcohol is the main cause of chronic pancreatitis in Taiwanese, and chronic pancreatitis increases the risk of pancreatic cancer. Overall, pancreatic cancer is difficult to diagnose early, and there are no clear specific risk factors. In addition, the prognosis is not ideal, so it is called the king of cancer for a reason.
What are the possible symptoms of pancreatic cancer? Are the location and symptoms different?
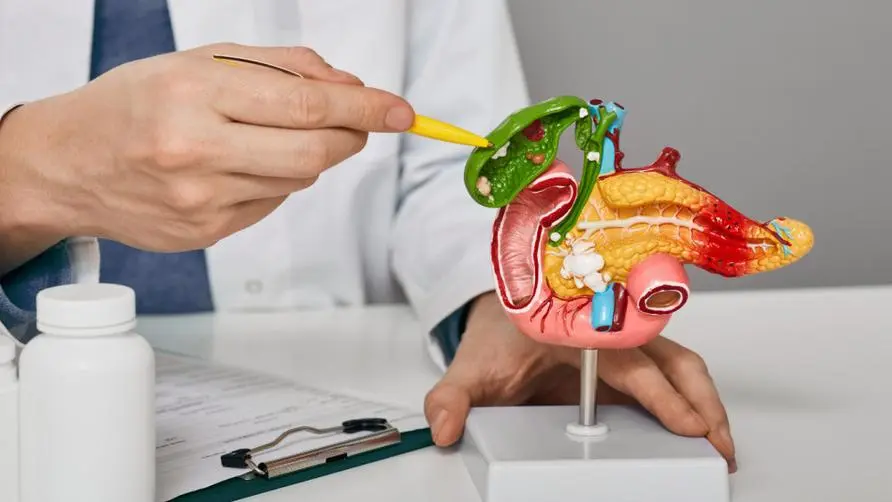
The pancreas looks like a long curved measuring stick and can be divided into three parts: the head, body, and tail of the pancreas. The head of the pancreas is larger and hook-shaped, and the body and tail of the pancreas are ruler-shaped. The head of the pancreas is the part where the pancreas and the duodenum are connected. Most of the pancreatic juice of the pancreas is connected to the common bile duct through the main pancreatic duct and opens at the large papilla of the duodenum. The tail of the pancreas is connected to the spleen.
Since the head of the pancreas is located at the crossroads where the common bile duct and the main pancreatic duct meet, its pancreatic juice components are mainly exocrine enzymes including trypsin, pancreatic lipase and other digestive enzymes. When the tumor grows in the head of the pancreas, it will block the common bile duct, preventing bile from flowing, causing jaundice of the skin and eyes, dark brown urine, and grayish white feces.
When pancreatic cancer grows in the body and tail of the pancreas, it does not block the bile duct and has no obvious signs. Most of the cancer will grow to a considerable size and even invade peripheral blood vessels and nerves, causing late-stage cancer symptoms such as abdominal pain and weight loss. ,thin. Patients may also experience a loss of appetite or continue to have pain despite treatment for stomach problems and gallstones. Relatively speaking, tumors occurring in the head of the pancreas are more likely to be detected early, while tumors in the body and tail of the pancreas are mostly at an advanced stage or have metastasized to the internal organs when diagnosed.
What are the screening methods for pancreatic cancer? Who is in the high-risk group?
The pancreas is located in the posterior abdominal cavity and is shielded in front by organs such as the stomach and intestines. The intestinal cavity is filled with air and cannot be penetrated by ultrasound. It is the most difficult organ to examine among all internal organs. Currently, the more effective pancreatic examination tools are computed tomography and more advanced MRI. However, computed tomography scans involve a certain amount of radiation and require relatively high equipment and examination costs, making them less suitable as a universal screening tool.
Another examination tool is “endoscopic ultrasound”, but the examination requires gastroscopy, which is an invasive examination and the patient will feel a certain degree of discomfort. It is usually used as a differential diagnosis in cases of suspected pancreatic cancer. As for the whole-body positron scan, its principle is to use radioactive isotopes to mark areas where cells gather with strong metabolism. It is often used for cancer tracking or to determine the extent of tumor metastasis and spread.
According to research from Johns Hopkins University in the United States, high-risk groups for pancreatic cancer include: family history (especially immediate relatives) of pancreatic cancer, a history of chronic pancreatitis, and unexplained acute pancreatitis in older people. etc., there is an opportunity to detect earlier pancreatic cancer through early screening. The most commonly used examination tool today is to draw blood to detect the tumor indicator CA19-9. The value for ordinary people is below 37, but for patients with pancreatic cancer, the value may be as high as tens of thousands or more than 100,000. However, limited by the specificity and sensitivity of tumor indicators, ultrasound and computed tomography scans are still required for further differential diagnosis.
What are the latest treatment trends for pancreatic cancer? How effective is surgery and chemotherapy?
Pancreatic cancer is a solid tumor, and the standard treatment is surgical resection. Pancreatic cancer can usually be divided into three situations when it is discovered. The first situation is that it has not metastasized and the location is suitable for surgery, but clinically the proportion of this type of pancreatic cancer is very small; the second situation is that it has metastasized to other internal organs in the abdominal cavity. , is no longer suitable for surgery; the third situation includes borderline resectable or locally unresectable tumors that have not spread to the liver or lungs but have lymphatic metastasis.
Most pancreatic cancers are inoperable or difficult to remove when they are discovered. Some tumors are even covered in the abdominal blood vessels, making surgery extremely difficult. The average proportion of patients who can undergo surgery is less than 15%. Most patients require systemic treatment including chemotherapy, electrotherapy, immunotherapy, and cell therapy. However, the five-year survival rate is generally less than 10%, and it can be done when the tumor size is small. Metastasis occurs, and once it recurs after surgery, it is usually ineffective in responding to drugs, and the therapeutic effect is limited.
For pancreatic cancer tumors that are inoperable or borderline resectable, the latest treatment method is to shrink the tumor through a period of chemotherapy to increase the chance of being operable. Nowadays, various chemotherapeutic drugs have different mechanisms of action. They inhibit DNA synthesis, inhibit cancer cell replication, and target the immune system. Through combined treatment with different chemotherapeutic drugs, there is an opportunity to shrink the tumor and gain the opportunity for another surgery. .
Is there any chance of early prevention of pancreatic cancer? Can eating less high-sugar foods help?
The clear cause of pancreatic cancer has not yet been found. To prevent pancreatic cancer, you should first understand whether you belong to a high-risk group, whether you have long-term drinking, chronic pancreatitis, or sudden acute pancreatitis. In addition, many patients with pancreatic cancer are newly diagnosed with diabetes two or three years before diagnosis. It is currently believed that diabetes is related to pancreatic cancer and is also a risk factor that needs attention.
Taking a comprehensive look at the risk factors related to pancreatic cancer, such as family history, diabetes, and obesity, they are all related to genetics. In addition to quitting smoking, abstaining from alcohol, and controlling weight, those who are themselves at high risk are recommended to regularly consult a gastroenterologist and receive relevant examinations. Increases chances of detecting cancer early. In addition, developing the habit of regular exercise can also help reduce the risk of cancer.
Nutrients and pharmaceutical ingredients that current scientific evidence shows can help prevent cancer include: vitamin C, low-dose aspirin, Statins, and the hypoglycemic drug Metformin, all of which can help reduce pancreatic cancer to a certain extent. Please seek medical advice before use. Specialist evaluation. In terms of diet, drinking alcohol can cause chronic pancreatitis. The drinking age of Taiwanese people has dropped and the number of clinically diagnosed pancreatic cancer cases among young people has increased. Reducing or completely avoiding alcohol intake is also an important consideration in preventing pancreatic cancer.
Further reading: