When you are left with only a respirator to accompany you, stress syndrome may come quietly! How can people who have recovered from COVID-19 get out of the shadow of diagnosis?

In May this year, the COVID-19 epidemic severely shocked Taiwan. After two and a half months of concerted efforts by the people, the epidemic gradually slowed down and the level of alert was lowered from level three to level two. However, while all industries are recovering, the mental health of a group of people is in jeopardy - they are recovered COVID-19 patients. Foreign studies show that 32.2% of those who suffer from COVID-19 and are seriously ill will develop post-traumatic stress disorder (PTSD); 14.9% will have depression symptoms; and 14.8% will have anxiety symptoms. You may be wondering, why do you have so many psychological problems after recovery? Let us take a look at the conditions experienced by recovered patients during the epidemic. Perhaps we will be able to better understand their mood and know how to help them.
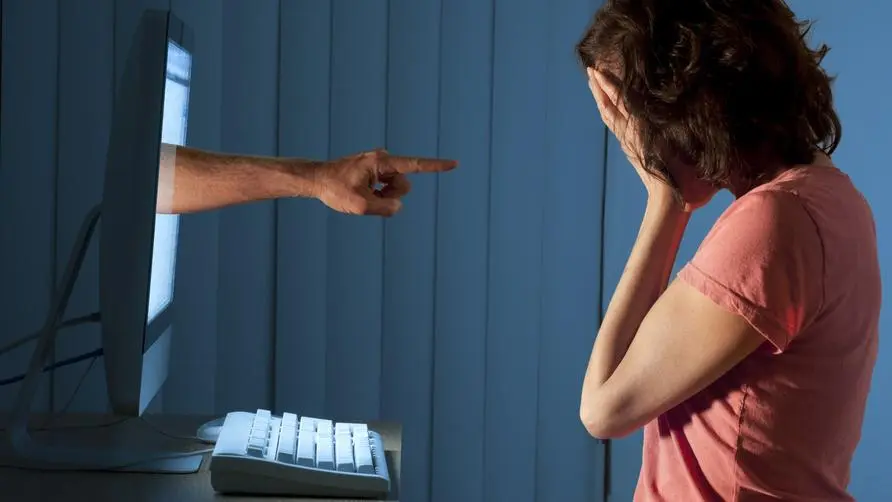
When only respirators are left around, it puts huge pressure on patients in isolation
During the isolation period in the hospital, the patient may only encounter medical staff during meal periods, X-ray photography, examinations, and consultations. The rest of the time, the patient will be alone in the ward. Let’s try to think about it, if we have a fever, cough, difficulty breathing, wear a respirator, lose our sense of smell and taste, and are in a strange environment without anyone by our side, would we feel scared? Therefore, for several weeks The fear and insecurity will cause huge psychological pressure on patients in isolation.
Just because you’re discharged from the hospital doesn’t mean you’ll be fine! Recovered patients may suffer from the following symptoms
Even after recovery and discharge, recovered patients may experience the following symptoms:
1. Post-traumatic stress disorder symptoms
Post-traumatic stress disorder (PTSD) is a serious mental illness. Traumatic situations will frequently and suddenly invade the mind. For example, while cooking, the mind suddenly flashes back to the scene when one is intubated. Some people may even feel the smell, the touch of the tube, and the infarction that makes them unable to speak. The situation is real. It’s scary.
Secondly, patients will avoid things related to traumatic situations. Some people will be afraid to hear the news about COVID-19; afraid to go to the hospital; afraid of confined spaces; afraid of being alone. Due to the tightness of being hospitalized for a long time, the sympathetic nervous system will be over-activated, causing the patient’s level of alertness to increase significantly, and it is easy for the patient to be frightened by external stimuli, such as the sound of a door closing or stationery falling to the ground. frightened.
Continuous nightmares at night will also deeply trouble the recovering patients. The recovering patients I took care of once told me, “I often dream about returning to the isolation ward. I scream in fear in my dreams and want to leave the room, but I can’t do anything.” I couldn’t open the door. The nightmares really made me afraid to fall asleep. I often couldn’t tell if it was a dream or if I was actually back in the ward."
2. Anxiety symptoms
Anxiety can make people restless, and when talking to the patient, they may seem to be speaking quickly and irritably. Difficulty concentrating can also deeply trouble patients, causing others to think that the patient’s answers are incorrect and often find it difficult to match the frequency. Anxiety is also easily accompanied by muscle tightness, irritability, sleep problems, and other physical symptoms, such as heart palpitations, dizziness, weakness, etc., but no obvious physical lesions can be detected.
3. Depressive symptoms
Depression will slow down everything from thoughts to movements. When talking to the patient, you will feel that the patient’s whole body has become very slow, and the speed of speaking and thinking has slowed down. At the same time, he becomes depressed, depressed, and loses his energy. My thoughts have also become more negative than before, and I often blame myself and think that I have not done well enough. I feel depressed all day long, lose interest in leisure activities that I used to like, and don’t really want to communicate with others.
The lingering shadow of recovery from a serious illness can help ease the psychological state by sincere companionship
How to help friends and relatives after recovering from COVID-19:
1. Understand deep thoughts
When recovered patients go home from the hospital, they often worry about whether they will infect others again. There have been recovered patients who washed and disinfected their hands repeatedly after returning home due to excessive fear of infecting their families, resulting in peeling and injuries on their hands. Recovered patients will also worry about whether they will be infected again. Some people will excessively avoid people, public, and social situations, and slowly lose interpersonal relationships and fall into a state of isolation.
2. Sincere emotional support and listening
It can be seen from the above that even if the recovered patients are discharged from the hospital, they will still be in a state of fear and worry. Therefore, accompanying them and using a gentle attitude to care about whether the patient’s daily needs and supplies (food, medicines) are sufficient during the period of independent health management will be the first step to stabilize the patient’s mood. Secondly, after settling into the environment, the recovering person will gradually feel tired and fragile, and feelings of sadness, worry, and fear will also emerge. At this time, they will need the sincere care of friends.
When listening, it is recommended to use the “fear of infecting others” and “fear of reinfection” mentioned in the first point to talk to them, and try to express their emotions in the process. For example, “When talking about how to maintain family epidemic prevention, I feel that you are afraid of infecting your family, and I feel that you are very uneasy and worried.” “When talking about washing hands repeatedly, I feel that you are afraid, will you? Are you worried about being infected again?”, “When you just talked about your experience of using a respirator, you sounded a little scared. Can I listen to you more?”. When the emotions and thoughts hidden in the heart are spoken gently by trusted relatives and friends, the emotions will find an outlet to vent, and the mood will be much more relaxed.
3. Accompany medical treatment
Sometimes, mental illness caused by psychological stress is more serious than we think. If your relatives or friends still have symptoms of depression, anxiety, or post-traumatic stress disorder despite your support, it is recommended to seek medical treatment at a professional mental health clinic. For those who have recovered, it is very difficult and tiring to have to go to see a doctor just after being discharged from the hospital. Therefore, it is recommended to use gentle and patient persuasion and accompany the patient to a professional mental health clinic for help, which will greatly increase the patient’s willingness to seek medical treatment.
Any accident or illness may cause mental injury, but your warmth and listening can speed up the psychological recovery of the recovering person. We look forward to working together to care for our relatives and friends who need help after the epidemic, and let society move towards the road of recovery.