Detailed explanation of hemorrhoids! See symptoms and treatments at once! Who are the high-risk groups? Does the surgery have to be painful?

What disease is hemorrhoids? How to distinguish internal hemorrhoids from external hemorrhoids?
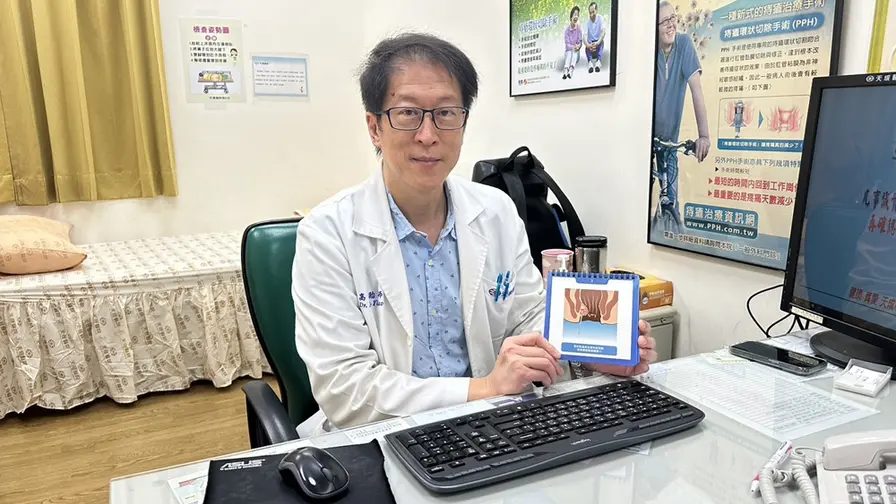
Hemorrhoids are composed of small blood vessels including arteries and veins, connective tissue, and small smooth muscle fibers in the anal opening. Hemorrhoids that occur above the dentate line of the anus are called “internal hemorrhoids”. Hemorrhoids that occur below the dentate line of the anus and outside the anal opening are called “external hemorrhoids.” Internal and external hemorrhoids that occur at the same time are called “mixed hemorrhoids.” Most hemorrhoids are mixed. hemorrhoid.
Hemorrhoids are considered the “anal cushion” of the human body, which can maintain the tension of the anus and help seal the anal opening. Hemorrhoids are most common in the right front, right back, and left sides. When there is pressure around the anus, such as increased pressure in the anorectum caused by prolonged sitting, it may cause the elasticity of the connective tissue of the anal cushion to weaken, causing excessive tissue proliferation and slipping out. In severe cases, internal hemorrhoids may even fall out of the anus due to prolapse.
Who are at high risk for hemorrhoids? Is physical stress the main cause?
“Intra-abdominal pressure” and “physical constitution” are the main causes of hemorrhoids. Modern people lead a stressful and busy life, coupled with changes in eating habits and difficulty in defecation, are all reasons for the increased incidence of hemorrhoids. According to statistics, the prevalence rate of hemorrhoids in Taiwanese people is estimated to be as high as 30%, especially among those aged 45-55 years old.
In addition, factors that easily increase intra-abdominal pressure, such as work patterns that require long periods of sitting and standing, pregnancy, poor defecation habits, excessive exertion, irritating foods, and low fiber intake are all considered to be related to the occurrence of hemorrhoids.
What are the symptoms of hemorrhoids? Don’t hold back the anal pain due to bleeding?
Bleeding, anal pain, hemorrhoid prolapse, and anal itching are the four most common symptoms of hemorrhoids. Generally speaking, internal hemorrhoids will not cause obvious pain. The most common symptoms of internal hemorrhoids are bleeding and hemorrhoid prolapse. Bright red blood stains may appear before and after defecation and will not mix with the stool.
In rare cases, chronic blood loss from ruptured internal hemorrhoids may also cause anemia. In addition, itching and oozing of stool around the anus may also be caused by hemorrhoids, which may even cause mild fecal incontinence, or mucus and secretions leaking around the anus, causing a feeling of moisture or fullness in the anus.
Compared with internal hemorrhoids, external hemorrhoid thrombosis is more common, and may be caused by stagnant blood clots. This “thrombotic hemorrhoid” is the most common external hemorrhoid that causes anal pain. It not only causes acute pain, but also has an obvious “lump” that can be touched. , it will continue to bleed when it ruptures.
Diagnosis and staging of hemorrhoids? If you can’t push it back, does it mean you have prolapse?
When bloody stools, anal itching or acute anal pain occur, other possible causes such as anal fissures, ulcers, polyps, malignant tumors, etc. must be ruled out. Or the hemorrhoids have prolapsed outside the anus and can be diagnosed visually. Usually thrombosed hemorrhoids are very painful when palpated, and anoscope and internal examination may also be required to assist in judgment. Generally speaking, internal hemorrhoids are divided into four levels according to their severity:
First degree: Hemorrhoidal tissue proliferates in the anus without prolapse.
Second degree: Hemorrhoid tissue proliferates and protrudes out of the anus during defecation, but can retract on its own after defecation.
Third degree: The hemorrhoids will protrude outside the anus during defecation and cannot retract on their own, so they need to be pushed back by hand.
Fourth degree: The hemorrhoids are completely prolapsed and cannot be retracted or pushed back.
What is the treatment for hemorrhoids? Does surgery definitely need to be performed?
Drug treatment: hemorrhoid ointments, suppositories, oral medications (stool softeners and anti-inflammatory analgesics). Anal plugs can be used for first-degree internal hemorrhoids that occasionally bleed without prolapse. Second to third-degree internal hemorrhoids may retract. Suppository treatment may also be considered.
Hemorrhoid surgery: After conservative treatment, it still affects daily life. If there is repeated bleeding, third to fourth degree hemorrhoids combined with prolapse, or ulcers, anal fissures, vaginal canals, or hyperplastic polyps, surgical treatment must be considered. The main surgical methods include traditional internal and external hemorrhoidectomy surgery, energy device minimally invasive hemorrhoid surgery, and newer laser hemorrhoid ablation surgery. Other surgical options include circumferential resection and artery ligation.
Traditional hemorrhoidectomy: Electric cautery or scissors are used to completely remove the internal and external hemorrhoidal tissue. It usually requires semi-general anesthesia and hospitalization for 2 to 3 days after the operation. It can effectively eradicate internal and external hemorrhoids and reduce recurrence. The disadvantage is that the wound is more painful after the operation and needs to rest for about a week.
Energy device hemorrhoid surgery (minimally invasive): Use energy devices such as tissue coagulation knife or ultrasonic knife to perform surgery. The scope of surgery is equivalent to that of traditional hemorrhoidectomy. It causes less thermal damage to tissues. At the same time, because of its good hemostasis effect, it can reduce the need for sutures. Hemostasis, postoperative pain is lower than traditional methods, and wound recovery is slightly faster.
Laser hemorrhoid ablation surgery: A laser probe is used to puncture and insert the affected part of the anus, and then a bipolar infrared laser is used to ablate the hemorrhoidal tissue. The puncture needle hole in the wound is too small, and the postoperative pain is almost painless. It is most suitable for patients with bleeding internal hemorrhoids and severe prolapse, but external hemorrhoids are large in size or combined with excess skin and still need to be removed and trimmed.
After surgery, you should pay attention to the frequency of going to the toilet to avoid the wound being stretched or the surrounding tissue edema. For post-operative anal hygiene, it is recommended to take a sitz bath or use a pad to help absorb blood oozing. On weekdays, you should pay attention to the prevention methods of hemorrhoids, including drinking more water, eating more fruits and vegetables, staying up less late, developing regular defecation habits, not sitting or squatting on the toilet for long periods of time, and flushing the anus with warm water to reduce irritation.
Further reading: